For the better part of the 20th century, the inventions and business ventures of the Industrial Revolution powered the U.S. and other advanced countries to levels of prosperity never seen before.
But in the 1970s and 1980s, the upward momentum of progress started slowing, grinding down to a much more sluggish pace. While the national average income -- gross domestic product (GDP) per capita -- continues to expand, the real growth rate has slowed from 2.4% per year in 1929-1979 to an average of 1.7% since 1980, including a growth rate of only 1% since 2007.
So what explains the slowdown?
Living standards increase when the quality of goods and services increases relative to the costs of producing and distributing them. Historically, huge jumps in the quality-to-cost ratio were apparent in fields like power (think electricity), transportation (railways, and then autos and airplanes) and communication (first telegraph, then telephone, internet and smartphone).
But certain large sectors of the economy are suffering from something like reverse-innovation: Costs are increasing much faster than any incremental improvement in quality.
In ║┌┴¤═°'s new report with the U.S. Council on Competitiveness, I argue this is happening in healthcare, housing and education.
Take healthcare. From 1980 to 2015, healthcare expanded from 9% of the national GDP to 18%. Some of this is natural and good. The aging population requires more healthcare, and even modest economic growth has freed up spending power for healthcare. The problem is that the per-unit costs of healthcare -- actual procedures, visits with doctors, pharmaceuticals -- have all soared. So the question must be asked: Has it been worth it?
I conclude not.
One way to evaluate advances in healthcare is to compare new treatments with the current standard treatments (e.g., how a new fever-reducing drug compares with ibuprofen) in terms of both costs and effects on "quality-adjusted life years." University of Chicago economists for every healthcare advancement analyzed in medical journals since 1976. The results suggest that the quality-to-cost ratio has fallen. Most new treatments introduced since 1976 have lower benefits per dollar than standard treatments. Indeed, for typical treatments, quality advances were very modest (1%) but cost increases were substantial (8%).
One can see evidence of systemic healthcare inefficiencies in the general health of the U.S. population, which collectively is much lower relative to peers in other developed countries despite the U.S. spending about twice as much on healthcare on a per capita basis. Mortality rates, which remain high by international standards, have fallen since 1980, but most of the progress has occurred among infants and the elderly. The working-age population has seen little improvement -- and for whites and American Indians, there have been no gains in age-adjusted mortality for people aged 15 to 64, at least since 1999.
Even as Americans are living slightly longer, the quality of life hasn't necessarily improved for people of working age. For U.S. residents, self-reported health status has fallen among each age group between 25 and 59 since 1990.

Additionally, the share of the working-age population suffering from a disability that prevents them from working rose from 4.4% in 1980 to 6.8% in 2015, adjusting for age.

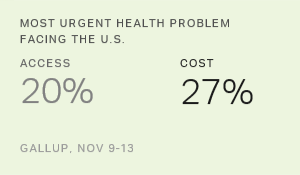
Inefficiency of Healthcare Looming as Crucial Problem
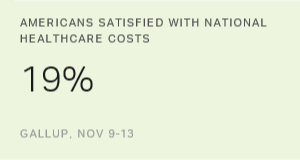
One reason for the decline in Americans' self-reported health status is the extraordinary inefficiency of the U.S. healthcare system.
It may be tempting to dismiss these poor health outcomes as driven by cultural or demographic changes, but the broadest evidence suggests this would be misleading. The fastest-growing minority groups -- Hispanics and Asians -- are typically healthier than whites and blacks. Moreover, compared with 1980, Americans are , smoking less and eating somewhat , and they are less likely to be abusing drugs and alcohol. The exception is the rise of prescription opioid use and related abuse, but our healthcare system bears much of the blame for that.
On the cost side, it is easier to identify specific causes for rising inefficiency.
Administrative costs related to healthcare billing are astronomical ( annually) -- especially compared with other advanced countries, where single-payer systems streamline procedures. Compared with their Canadian counterparts, nurses in the U.S. an extra 18 hours per week on administrative tasks and clerical workers spend an additional 37 hours. , Medicare started requiring that medical service providers identify the specific diagnostic code (out of roughly in the latest system) to get reimbursed. Complicating matters more, Medicare and private insurance companies have different billing, documentation, and submission rules and procedures, making it extremely difficult to create efficient software.
Even without a single-payer system, Congress could reform the medical billing system with the goal of creating a simplified, universal, digital process. The goal should be to require only the minimum information that is necessary to avoid fraud. Reimbursement should be based on reasonable approximations of the actual costs to providers in terms of time and use of equipment, and the application process for providers to become a qualified biller of either private or public insurance should be streamlined.
Another issue relates to competition. Consumer advocates at the argue that state laws protect hospital monopolies and by blocking the introduction of competitors into the market, driving up costs by tens of billions of dollars. State licensing regulations restrict qualified healthcare providers -- like nurse practitioners and dental hygienists -- from practicing independently, as pointed out by the . Addressing these restrictions could reduce the costs of medical care.
There are other problems with the U.S. healthcare system. The complicated practice by which pharmaceutical companies develop new drugs and set their (often very high) prices continues to come under scrutiny and provides the opportunity for potential reform. Likewise, agencies are to explicitly recommend or deny public funding for treatments based on the most widely used quality-to-cost comparisons.
The overarching point is that the absurd inefficiency of U.S. healthcare is not necessary or permanent. The system we have now is harming us through its exorbitant costs and weak efficacy, which drive down economic growth and deprive future generations of greater prosperity.